Designing a Mobile Patient Information Sharing System using Patients Community Members: Perceptions of Emergency Physicians
2 Kyoto University Hospital, Kyoto, Japan, Email: kuhp.kyoto-u@ac.jp
3 Graduate School of Medicine, Kyoto University, Kyoto, Japan, Email: kuhp.kyoto-u@ac.jp
Received: 25-May-2020 Accepted Date: Jun 09, 2020 ; Published: 16-Jun-2020
Citation: Morris K, Yamamoto G, Sugiyama O, Luciano HO. Santos LHO, Tsutsumi T, Ohtsuki R et. al. (2020). Designing a Mobile Patient Information Sharing System using Patients Community Members: Perceptions of Emergency Physicians EJBI 16(2): 01-09
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact submissions@ejbi.org
Abstract
Objectives: Emergency Physicians utilize multiple patient information (PI) sources within Emergency Departments. Access to a centralized health record system is ideal but not always available to physicians. A technological gap exists in the context of PI sharing regarding patients’ representative and their in-situ involvement as an alternative PI source. The purpose of this study is to understand emergency physicians’ perceptions about patients’ representative and our design concept for improvement of PI sharing to physicians.
Methods: Observations focused on physician’s interaction with representatives were used to understand the emergency setting which led to a mobile PI sharing application design. Semi-structured interviews were conducted with three experienced physicians to obtain their perceptions about the usefulness of our proposed design.
Results: Physicians shared their experiences about interactions with patient representatives and perceptions about potential use our proposed design concept. Physicians’ main problems during interaction with representatives were insufficient PI and occasional unfavorable attitudes. Regarding our design concept, physicians’ perceived benefits were reduced information-seeking time, reduced PI search actions, and reduced stress. Physicians’ perceived shortcomings were related inter-department PI sharing features and insufficient PI relating patients’ daily activities prior to admission and a do not resuscitate policy.
Conclusion: Physicians are willing to use our design concept in the future if concerns about security, upto- date PI and PI reliability are addressed. Although our current design concept focuses on the point of interaction between physicians and representatives, our scope will be widened to consider inter-ED PI sharing features and event-based PI.
Keywords
mHealth, Information Sharing, Emergency Department, Representative Involvement, Patient Preferences
Introduction
Emergency Departments (ED) have unique characteristics in that emergency physicians need timely access to patient information (PI) to make faster informed decisions about treatment and diagnoses of patients [1]. An important responsibility of Healthcare Professionals (HCP) is the clinical care of patients; however, during some episodes of care, information seeking for PI as a non-clinical task occupies a considerable amount of their time [2-4], a challenge further compounded by the ED setting [5,6].
If patients are capable of sharing PI, physicians use minimal PIseeking time, thus dedicating more time to treatment and earlier diagnosis during episodes of care. In this paper, capable patients are considered to be those who can communicate and share their PI verbally or electronically with HCPs within an ED. In Japan, mhealth solutions such as the SHACHI system allow patients to share their clinical PI with third-party healthcare facilities [7].
In many cases PI is obtained through direct patient interviews and evaluation of the patient’s medical records through the Electronic Health Record (EHR) systems; efforts to improve PI sharing between capable patients and HCPs on a nationwide level have been reported [8]. However, other times it is necessary for HCPs to turn to other PI sources. Under some circumstances patient representatives become a primary PI source; they can share PI that is not limited to medical history, but also events that led up to the emergency situation [1]. Patient representatives have been referred as ‘family member’, ‘proxy’, ‘representative’ where they make decisions on behalf of an incapable patient [9-13]. In this paper, we define the patient’s representative as any entity which occupies an In-situ role of sharing PI with HCPs on behalf of a patient.
Physicians have benefited from improved information sharing during interaction with capable patients. However to the best of our knowledge, in the context of PI sharing, no study has focused on improving the information shared by patient representatives within the ED setting.
Healthcare facilities in Japan are divided into primary, secondary and tertiary levels [14,15]. We chose to base our study on a tertiary level ED within the aim of addressing the following research question: How do we improve the interaction between physicians and representatives?
In this study we focus on the patient’s representative, an information source that can contain various people who are assumed to have a close relationship with patients prior to an emergency situation.
The objectives of this study are as follows:
1. Deepen our understanding of physicians’ information seeking behavior and interaction with patient representatives.
2. Propose a conceptual design to improve interaction between physicians and patient representatives.
3. Gather emergency physicians’ perspectives about their experiences and opinions about patient representatives.
4. Obtain feedback from physicians about the proposed conceptual design outlined in objective 2.
The above objectives were achieved through conducting observations regarding physician acceptance of the concept design and semi-structured interviews focused mainly within the scope of physicians.
The remainder of this paper is outlined as follows. Section 4 briefly highlights the observations used to understand the ED context based on objective 1 and a clarification of the interaction problem between physicians and representatives. Section 5 presents a socially based design concept focused on physician’s interaction with patient representatives. Section 6 describes the interview used to gather feedback from physicians about the design concept along with results based on objectives 3 and 4. Discussions based on the findings are described in Section 6.
Observations
A 31-hour observation was performed at an outpatient ED of a tertiary level hospital in Japan to gain more understanding about the PI information needs and information seeking behavior of physicians and their interactions with patient representatives. Permission was obtained from the ED management prior to the observations. One observer was involved in the observation stage.
Data Collection and Analysis
Five attending physicians were present during the observations with additional medical students, resident physicians and nurses. Informal interviews were done with physicians during the observation. Information behavior of physician and representative in the ED were recorded by hand-written notes. Although the activities of various HCPs were observed, our main scenario of focus was the situation where physicians could not access PI in the ED. The observation notes were then read multiple times for familiarization. After, the notes were checked to verify that no patient or physician identifiable notes were included. The notes were then imported into QDA Miner [16], a software tool used to code the observation notes. The focus of the analysis were scenarios where physicians interacted with representatives to obtain PI.
Summary of Findings
Half of admitted patients did not have their clinical PI available within the hospital (48.7%). Twenty-six patients arrived by ambulance (66.7%) and six were walk-in patients (15.4%). The arrival status of seven patients was undetermined by the observer (17.9 %). Physicians also tried to contact a remote colleague through repeated telephone calls, a similar practice reported in a previous study [17]. Physicians’ usage of available PI sources varied depending on the emergency situation. For example, a physician may use information from a patient’s family member to identify and contact the primary care facility. We focused admission and treatment stages of patients (Table 1). Apart from family members, some patients were accompanied by members of the healthcare community (nurses and caregivers). This finding led us to consider patient representatives as not just members of patients’ community but also the healthcare community since they interact with some patients on a day-to-day basis. Drawing from the observations, the following scenario served as a basis for our concept design in the following section:
| Role | Examples | Patient Journey | ||||
|---|---|---|---|---|---|---|
| 1. Admission | 2. Treatment | 3. Diagnosis | 4. Transfer | 5. Discharge | ||
| Clinicians | Physicians | √ | √ | √ | √ | √ |
| ED Nurse | √ | √ | √ | √ | √ | |
| Administration | Support staff | √ | √ | √ | ||
| Care manager | √ | √ | ||||
| In-situ Representatives | Nurse | √ | √ | |||
| Caregiver | √ | √ | ||||
| Family member | √ | √ | ||||
| Relative | √ | √ | ||||
| Spouse | √ | √ | ||||
| Close friend | √ | √ | ||||
Table 1: Active persons and their roles during a patient’s journey based on our observations and discussions with physicians.
-An emergency situation where a patient is incapable of sharing PI with physicians in the ED. The patient’s representative is present in the ED and the attending physician requires PI but cannot obtain PI from the current information system in the ED.
The chosen scenario above formed the basis for the problem definition in this study. At least two physicians confirmed our assumption that PI shared by representatives is “useful but very limited”. The observation findings formed the basis for brainstorming ideas to improve the interaction between representatives and physicians in the ED.
System Design
We designed a mobile application system focused on admission and treatment stages of patients (Table 1); this design was done based on our observations and discussions with physicians. In the context of PI sharing, we focused on stages 1 and 2 where physicians interacted initially with patient representatives to obtain PI. During admission and treatment stages, physicians engage in extensive PI seeking behavior before a more informed diagnosis could be made during the diagnosis. Our design was based on the following hypotheses derived from observations and discussions with emergency physicians:
• Physicians will accept using the system for interactions with representatives if it is easy to use (DH1). A busy physician requires simple but effective interactions that can yield the required PI. We assume that during interaction with representatives, physicians will want to use our proposed system if it is easy to learn and use.
• Physicians will accept the proposed system if it seamlessly supplements the current interaction process that occurs between physician and patients’ representatives (DH2). Since the ED setting has many stressful situations, introducing a new system should not add additional non-clinical tasks to physician’s workload [18].
The remainder of this section presents a conceptual explanation of the elements that contributed to the mobile application design.
Involving Community Stakeholders
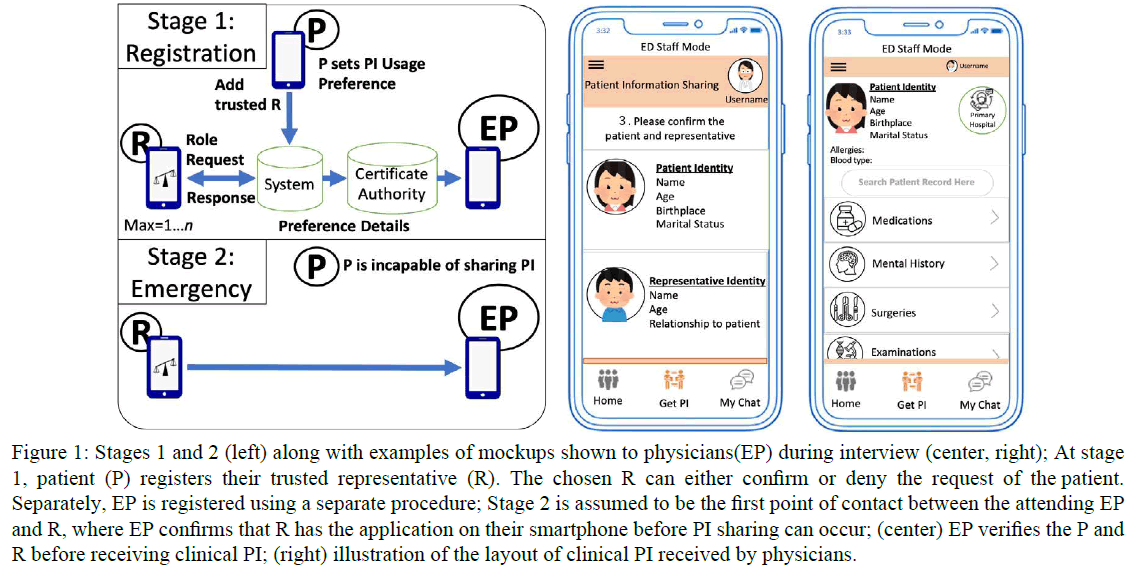
The system design is patient-centered since a patient determines who will be added as a representative. The patient will also choose what the representative can do with their information (Figure 1). In our research, after discussions with emergency physicians, the following states deem a patient to be incapable [19] in the context of patient information sharing:
Figure 1: Stages 1 and 2 (left) along with examples of mockups shown to physicians(EP) during interview (center, right); At stage 1, patient (P) registers their trusted representative (R). The chosen R can either confirm or deny the request of the patient. Separately, EP is registered using a separate procedure; Stage 2 is assumed to be the first point of contact between the attending EP and R, where EP confirms that R has the application on their smartphone before PI sharing can occur; (center) EP verifies the P and R before receiving clinical PI; (right) illustration of the layout of clinical PI received by physicians.
1. Unconsciousness based on Glasgow Coma Scale or Japan Coma Scale,
2. Inability to speak,
3. Inability to speak and move,
4. Psychological disorders and
5. Mental state where conscious judgement is impaired, e.g. alcohol intoxication.
HCPs require an efficient and secure way to obtain PI that requires the least possible effort since searching for PI is not the core of the treatment and diagnosis process [20]. We assumed that as the capacity of an ED increases, the problem of continuous searching for PI that cannot be accessed through the system in the hospital will increase. Hospitals provide facilities for physicians to treat patients and has various technological tools [21] to support physicians and other HCPs. Since the PI has to be viewed on a device that is managed by the hospital, hospitals must be included at the system design stage.
Within an in-situ role, representatives will share PI if the patient is incapable. The representative is seen as someone the patient trusts (family member, friend care- giver, close friend), and this role of acting on behalf of the patient is considered to be a vital subset of the patient community. In the context of PI sharing, the healthcare and patient community are combined into one in-situ role, the patient representative.
System Stages
Registration Stage: In this system design, a patient’s active role is during the registration stage before an emergency situation occurs (Figure 1). The necessity of this stage was considered based on recent changes in focus of healthcare systems to being patient-centered, with patient wanting more control over their clinical PI [22,23], with the support of relevant authorities [24]. A patient is assumed to want granular control over some parts of their shared information, even during emergencies, as mentioned in our previous work [25]. At this stage, a patient adds a chosen representative. This representative can be a trusted family member, spouse, relative or close friend.
The mobile application used by physicians is assumed to be used on a smartphone which is owned by the hospital. Using a remote certificate authority described in [26], physicians are registered to reduce the risk of unauthorized physician registrations.
Emergency Stage: During the emergency stage, i.e. interaction between physician and representative, the patient is assumed to be incapable of sharing PI with physicians. If a patient is capable of sharing their PI, there is no need for the representative in our system. Based on the patient’s preferences, a representative shares PI with physicians. After PI is shared with physicians, the representative can revoke access rights based on patient preferences defined during the registration phase. In this system, the representative’s role does not allow them to see PI; they are able to share the information with physicians and revoke access to information depending on the access control features chosen by the patients prior to the emergency situation.
Personas and scenarios were created because the emergency setting is very unpredictable and has many situations; this strategy also allowed us to have a deeper discussion with physicians about the PI requirements of physicians using specific cases. Examples of screens physicians will see are illustrated in Figure 1.
Interviews
Semi-structured interviews are ideal for gathering the opinions of participants while simultaneously obtaining observational data to enrich data collection [27]. Interviews were done to achieve the following:
1. Clarify assumptions about observations mentioned in section 4.
2. Obtain deeper understanding of physicians’ perceptions about their experiences with patient representatives.
3. Gather feedback and understand perceptions of physicians about using the representative in our proposed sociotechnical system concept described in Section 5.
Study Design
Interview questions were designed in collaboration with two physicians whose feedback were used to refine questions to fit the understanding of physicians using the Japanese language. Two translators and one physician assisted in translating the interview questions to Japanese after iterative discussions with collaborating physicians. The interviews were designed in two parts, Before Concept Introduction (BCI) and After Concept Introduction (ACI).
BCI focused on the experiences and opinions of physicians about their interactions with patient representatives. Our goal in BCI was to understand physicians’ perceptions and attitudes about representatives based on their professional experience. There was no mention of the design concept in BCI and no hypotheses were created.
The aim of ACI was to obtain physicians’ perceptions and attitudes about the usefulness of our design concept in the ED and their willingness to use the proposed system in the future ED.
ACI was designed based on DH1 and DH2. Additionally, another hypothesis was created based on the observer’s understanding of the ED setting and discussions with collaborating physicians: physicians will be willing to use proposed concept in the future ED (EH1). During ACI, the design concept was explained, and mockups were shown to the interviewees (Figure 1). After the explanation, we gathered physicians’ opinions about the design concept and our inclusion of patients’ representatives within the concept.
Sampling and Data Collection
Purposeful sampling was used to recruit three physicians. Senior staff members were targeted since our goal was to obtain information about their experiences and opinions.
Two participants were interviewed face-to-face, and one was interviewed using a video conferencing platform. The online interview still followed the same interview process as the first two interviews. The type of questions used in the interview mainly focused on the experience, opinions and knowledge about their interactions with patient representatives. However, one question was asked about their feelings when they repeatedly searched for PI; this question was based on based on the observer’s findings.
Analysis
For qualitative analysis of the interview notes, we began with reflection of the interviews and checked the data. The data were then read multiple times for familiarization. Two native Japanese, one informatician and one physician, transcribed and translated the interview recordings before deeper analysis began.
Inductive analysis was used for BCI responses to identify common themes. Deductive analysis was used to analyze the ACI responses based on the proposed hypotheses (DH1, DH2, and EH1) mentioned in section 5.1. Afterwards, themes were identified using inductive analysis for ACI questions.
To check for reflexivity in writing, reflection about the coding process and interpretation bias was conducted [27].
Results
Three emergency physicians were interviewed. Each participant had 10-15 years’ experience in the ED setting. Interviews lasted on average 1 hour and 15 minutes. Physicians sometimes referred to a patient’s representative using the term, “key person”; one physician explained ‘key person’ as “someone who makes the main decisions on behalf patients with or without coordinated input from other family members”.
Before Concept Introduction
BCI mainly highlighted problems physicians experience relating to the patient representative. Problems were placed into three themes (Table 2); these problems mentioned by physicians during interaction with representatives were based on their experience in the ED.
| Themes | Quotes |
|---|---|
| During Interaction | "Sometimes family members are unfriendly" (physician 1) "[Interacting] face-to-face"doesn’t make sense if the person [representative] does not have PI" (physician 1, similar statement by physician 2) "Even if we were to talk to someone who doesn’t know better, sometimes the information we get turns out to be wrong information." (physician 2) |
| Perceived Causes | "If patients and their representatives are not on good terms, the family member,
although having enough information, sometimes do not want to share with us.
(physician 1) "We [physician and colleagues] were told that they [patient] had no medical history, but in fact they did. It comes down to not being able to get reliable information" (physician 2) |
| Impact of Problems | "For unconscious patients cases it is difficult to get their [patient] medical
information, so we must do more tests" (physician1, similar statement by
physician 3) "The lack of understanding of the medical background and the DNR policy is quite a problem. When it’s an emergency, decisions are made in a hurry, so the lack of this kind of information can affect decision making. It is a burden for us to check with the family member while performing the treatment in such cases" (physician 2)"We have to use more time and effort to get patient information, which affects the amount of time we have to treat the patient" (physician3, similar statement from physician 1) " After [a] patient was exposed to poisonous substances, it is necessary to wear an personal protective equipment while attending to a patient, however we were not aware of the danger..." (physician 3) |
Table 2: BCI Themes relating to problems experienced by physicians in the ED relating to the patient representative.
During Interaction: Physicians commented that the behavior and attitudes of some representatives during interaction made the task of getting PI much more difficult. In most mentions of this theme, physicians were referring attitudes that did not seem like the representative was willing to cooperate with physicians. One physician mentioned that “some family members are unfriendly”, and this problem makes interacting with these family members a more difficult task for physicians. Unfavorable behaviors relate to actions of representative that made PI information seeking difficult, “during an emergency, a patient’s close friend returned home with the patient’s belongings. Upon regaining consciousness, the patient was also unwilling to share information”. Despite unfavorable attitudes, physicians highlighted in- stances when patient representatives assisted physicians in searching for and/or provide missing patient information; one physician recalled, “the most recent experience I had was where a mother brought the relevant history of the child and had a positive attitude during our interaction. The support from her was really helpful”. Each physician shared the sentiment that patient information shared by representatives was, although useful, not sufficient. Apart from the general consensus about this problem, one physician also commented about the incorrect PI sometimes shared by representatives.
Perceived Causes: One cause mentioned by physicians for insufficient PI shared during interaction was patient- family tensions which preexisted patients’ arrival; this cause also affected the attitudes of representatives during interaction, sometimes leading to unwillingness to share PI. Patients sometimes withheld PI from their representative, who was willing to share PI that they were aware of at that time; one instance was recalled by a physician, “There was a case of an unconsciousness patient. We did many kinds of tests but we didn’t know the cause. Finally we detected the cause was drug overdose. The patient kept his medical history and drug history from his family”. However although knowing PI, patient representatives in other instances, withheld sensitive PI (perceived as shameful) from physicians. Physicians mentioned that misinformed representatives were people who thought that they had the right PI when in fact, the PI was inaccurate. For example, one physician commented that “we [physician and colleagues] were told that they [patient] had no medical history, but in fact they did. It comes down to not being able to get reliable information”.
Impact of Problems: Physicians also commented about the consequences of the above problems. Physicians mentioned that additional resources are used as a result of insufficient PI; this sub-theme relates to both human resources and medical supplies available in the ED. Additional PI seeking was also a sub-theme that came up during the interviews; this was mainly attributed to insufficient/unreliable PI. All of the above problems lead to higher stress levels among physicians who had to engage in the nonclinical task of additional searching for PI; “In the busy ED, my stress level gets higher especially when dealing with patients with circulation and respiratory problems”. Physicians mentioned the feelings of “frustration, anxiousness and desperation” when searching for PI within and outside of the ED.
Increased risks to physicians and their colleagues were mentioned by one physician based on insufficient PI which can be caused by withheld information. Furthermore, insufficient PI leads to misinformed treatment decisions and greater uncertainty among physicians about a possible change in patients’ future condition. For example, a physician mentioned that“ if they [patient] have diabetes and they feel pain in a certain area, if we know PI, we can predict from their historical patterns that they will probably have a myocardial infarction“.
After Concept Introduction
Physicians shared opinions about mainly their perceptions of the proposed system and the use of the representative in this system. Themes for the ACI stage were mainly related to perceived benefits, perceived shortcomings and concerns about using the proposed application system designed in section 5, as shown in Table 3. Two physicians expressed interest in using our proposed system in their personal lives while one physician took a neutral standpoint but open to trying to system in the future.
| Themes | Quotes |
|---|---|
| Perceived Benefits | "This system eliminates my need to wait on a physician to type summaries [in a
patient’s primary hospital]" (physician 1) "The sharing of patient information is fast and somewhat comprehensive" (physician 2) "The system is useful although it really depends on the quality of information received"(physician 3) |
| Perceived Shortcomings | "It seems difficult to reserve all medical data. I want to reserve [patients’] family
contact information, activity of daily living (ADL) and do-not-resuscitate (DNR)
policies." (physician 3) "There are no features to allow me to share PI with my colleagues in the ED" (physician 2, similar statement from physician 1) |
| Concerns | "When the representative is another person’s [another patient] representative
simultaneously, perhaps they can share the wrong information with medical staff."
(physician 3) "I think we need a separate person to manage patient’s data, such as who is responsible for editing the data and who is responsible for managing it." (physician 2) "I am concerned about information leaks and the correct timestamps for the [patient] information (physician1, similar sentiment expressed by physician 2) "Some older physicians do not own a smartphone, how will they use this system?" (physician 3) |
Table 3: ACI themes relating to physicians perceptions about proposed system design involving the patient representative.
Perceived Benefits Physicians highlighted several perceived benefits of using our proposed concept. With regards to reduced time, physicians remarked that using the system can reduce the time taken for them to request and obtain PI; this suggests that the system is perceived as easy to use by physicians, supporting hypothesis DH1. Concerning reduced searching, physician commented that using our system can help physicians “avoid the trouble of contacting the patient’s primary care facility”. Because of the proposed improvement to the interaction process with representative, a physician commented that the system can help him avoid “waiting on physicians in the primary care facilities of patients to write patient summaries”; this supports DH2 since physicians did not have any concerns about the interaction process with representatives using our system. With regards to reduced stress, a physician mentioned using our system can lead to “less frustration” since additional searching is not required to obtain PI. More Convenience relates to physicians’ thoughts about perceived convenience during interaction with patient representatives. One physician perceived our proposed design as “a better than just speaking to a family member”.
Perceived Shortcomings Physicians perceived our proposed system’s shortcomings based an explanation given to them and the mock-ups shown prior to ACI questioning. Perceived shortcomings were related to mainly the features and the target patient information included during the system design. Two physicians mentioned that although the system is useful, there was no feature presented to assist in sharing PI with other HCPs in the ED, after reception from the representative. The lack of a feature to support remote PI sharing was also mentioned by a physician. Concerning patient information physicians mostly mentioned the social background, Activity of Daily Living (ADL) and do not-resuscitate (DNR) policy as shortcomings of our proposed concept.
Concerns ACI Physicians had various concerns about the proposed system. With regards to PI, physicians were concerned about the management (information updates, reliability, and update transparency) of the clinical PI to be obtained prior to emergencies and after PI is received using our proposed system. Concerning information updates, a physician remarked that the information needs to be updated for any patient or the information integrity and usefulness of the system will be problematic. Information security (PI privacy, PI integrity) was also a concern. Concerning security, one physician mentioned that he had privacy concerns for patients, “If the physician can see [PI] but the friend [of the patient] cannot see, then the system is useful”. One physician was also concerned with the use of smartphones in the ED since many senior physicians may not be able to use smartphones efficiently and do not own a smartphone for personal or professional uses. Although the system was perceived as useful by all physicians, one physician also had concerns about reliability of PI obtained, which made him assume that additional PI seeking will still be needed after using our proposed concept. The capability of the representative to share PI was a concern highlighted by two physicians. Features designed for physicians were a concern for one physician who stated, “I don’t like the idea of the [proposed] system if [it is] connected to [my] personal information such as GPS (location information)”.
Discussion
In this study, we aimed to get a deeper understanding of emergency physicians’ interactions with patient representatives. Insights from the observations suggested that limited PI shared by patient representatives contributed to physicians’ additional PI-seeking behavior. The observations presented in section 4 allowed us to understand the ED setting and form a basis for our proposed mobile application design. Secondly, the proposed patientcentered design was done using insights from our previous work about patient preferences [25] and our observation findings. Our proposed concept allows patient representatives to have a technological option of sharing PI with physicians. Thirdly, we obtained physicians’ feedback about the proposed design concept using the patients’ representatives. Physicians are considered to be very important during the design process towards realizing our proposed concept in the future ED. Patient and representative perceptions are also vital, however, this study focuses on emergency physicians’ perceptions. Findings of this study suggests that physicians are willing to have an improved interaction with patient representatives in the ED, where more PI can be shared within a shorter time frame.
Findings
Physicians remarked that the system is perceived as useful in the ED. However, physicians also highlighted some shortcomings of the proposed system which serve as suggestions for improving our system design; two of such shortcomings were the lack of features for them to update and share PI and with other ED colleagues. The lack of a proposed feature to support remote PI sharing was also mentioned by a physician; although this feature was not included in our scope, this comment was very valuable and supports our remote PI sharing using patient representatives in our previous work [25]. Although intra-ED PI sharing is outside our scope at this stage, it is important to develop features to help physicians find meaningful use of PI obtained from representative. A physician also mentioned that “it’s not very good for anyone to write [PI] when you think about security. A trade-off between security and information updates needs to be considered.” physicians in a previous study expressed similar sentiments [28].
Results suggest that physicians are willing to use the proposed system during interacting with patients’ representatives, which supports DH1, DH2 and EH1. Based on the system mockups shown, physician mentioned that the system is perceived to be easy to use and helpful in reducing the task of searching for PI when they are very busy. However, one of the concerns mentioned related to the integrity of PI obtained using our system. Additionally, one physician was concerned about the wrong PI being shared by representatives; a possible solution can be the inclusion of a confirmation screen with a photo of the patient and representative so that physicians can clarify basic PI before clinical PI can be obtained from representatives (Figure 1). Results, although inconclusive, suggest that physicians would like to improve the interaction process with patient representatives by receiving not just assumed comprehensive and reliable PI, but up-to-date PI that includes a history of each HCP who made PI updates prior to an emergency situation.
Design Proposal
We consider physicians’ colleagues as part of the healthcare community and the patient and their representative belonging to the patient’s community; both communities are regarded as part of society with important roles. Within our design concept, we assume that a patient has at least one person they can trust to represent them during emergencies. The patient representative is seen as an extension of the patient in the system design, i.e. they must be assigned to a patient. Each stakeholder needs to be aware of their role(s) in the system before registration can be complete in stage 1. Additionally, intercommunity understanding is necessary to ensure the long term support and use of the implementation of our proposed concept in the future. Trust between the patient community and healthcare community is necessary to ensure that PI is available to physicians while considering the confidentiality of patient information [29].
In the future, to support the technical part of the system, is necessary that stakeholders have an understanding of the system at the registration stage to obtain meaningful use while maintaining patient privacy [30]. Insights received from experienced physicians will be used to update our system design prior to the development of a full-scale prototype.
Socio-technical approach
Patient’s representatives are very useful in the event either the patient or their PI is not directly accessible to the HCPs. Early principles about sociotechnical systems inspired our sociotechnical design of the proposed system [31]. Based on the Information Seeking Model reported by T. D. Wilson [32], we assume that the representative will be willing to share PI with physicians since the rewards for better patient care and physicians’ physical proximity in the ED are at a high level.
Within our system, patients can choose a trusted person to be their representative, but trust may change overtime. This is not a new limitation since traditional systems where one person represents the other is also prone to such a shortcoming. A patient-centered PI sharing system that is useful and usable to HCPs should be considered by including the perceptions of nurses and administrative support staff whose invaluable role contributes to continued patient safety.
Future work should include further validation and improvement of the system design to support intra-ED PI sharing after physicians receives PI from a patient’s representative.
Limitations
This study focused on establishing a social basis for the future development of a mobile PI sharing application with the involvement of patients’ representatives. Our scope was limited to experienced emergency physicians in one ED setting. The opinions of physicians and HCPs of other healthcare facilities were not included in this study. Thus, the findings of the observations and interviews cannot be generalized.
Conclusion
Emergency physicians utilize multiple patient information sources based on their PI needs. One information source not yet explored in the context of socio-technical patient information sharing is patients’ representative. This paper focuses on the physician’s perceptions using observations, system design and interviews to obtain a deeper understanding of physicians’ information requirements. We designed a mobile patient information sharing system to improve the interaction between physicians and patient representatives within the ED setting.
Semi-structured interviews with three experienced physicians revealed their experiences with patient representatives and their perceptions about using our proposed design concept. Physicians’ main problems during inter- action with PI were the attitudes of patient representatives and insufficient patient information. Physicians’ perceived benefits were related to reduce information seeking time, reduced PI search actions, reduced stress and more convenience when obtaining patient information. Physicians’ perceived shortcomings of our proposed system were related system features and target patient information that we did not consider during the system design stage. Physicians’ concerns about our proposed system were mostly related to the management, security and privacy of patient information. Despite the concerns, the proposed system was seen as useful by physicians, two of which are willing to use it as a patient in their personal lives as well as the future ED.
Physicians are willing to use the system in the future ED if the main concerns about security, information updates and information reliability are addressed. This study contributes knowledge about the socio-technical inclusion of patient representatives in the information sharing context and emergency physician’s perceptions about our proposed design concept. Technological support systems aimed at improving the social support for physicians are necessary; we believe that patient representatives can actively assist in that regard.
Acknowledgements
Special thanks to the emergency physicians who volunteered their time to share their experiences.
REFERENCES
- Ayatollahi H, Bath PA, Goodacre S. Information needs of clinicians and non-clinicians in the Emergency Department: A qualitative study. Health Information Libraries J. 2013; 30(3): 191-200.
- Finnell JT, Overhage JM, McDonald CJ. In support of emergency department health information technology. AMIA Annual Symposium proceedings/AMIA Symposium AMIA Symposium. 2005; 246-250.
- Cogdill KW. Information needs and information seeking in primary care: A study of nurse practitioners. J Med Library Assoc. 2003; 91(2): 203-215.
- Green ML, Ciampi MA, Ellis PJ. Residents’ medical information needs in clinic: Are they being met? Am J Medicine. 2000; 109(3): 218-223.
- Geisler BP, Schuur JD, Pallin DJ. Estimates of electronic medical records in U.S. emergency departments. PLoS ONE. 2010; 5(2): 5.
- Chacour BM, Shadmi E. Health information exchange and information gaps in referrals to a pediatric emergency department. Int J Medical Inform. 2016; 87: 68-74.
- Doi S, Ide H, Takeuchi K, Fujita S. Development of optin agreement and access control system for patients in a personal health record. Transactions of Japanese Society Med Bio Eng. 2017; 55(1): 45-49.
- Nøhr C, Parv L, Kink P, Cummings E, Almond H, Norgaard JR, et al. Nationwide citizen access to their health data: Analysing and comparing experiences in Denmark, Estonia and Australia. BMC Health Services Research. 2017; 17(1): 534.
- Prior SJ, Campbell S, Jane S. Patient and Family Involvement: A Discussion of Co-Led Redesign of Healthcare Services. J Participatory Med. 2018; 10(1): 5.
- Holliday CM. A Snapshot of Community Engagement in Research in the Context of an Evolving Public Health Paradigm: Review. J Participatory Med. 2018; 10(1): e1.
- Wendler D, Wesley R, Pavlick M, Rid A. Do patients want their families or their doctors to make treatment decisions in the event of incapacity, and why? AJOB Empirical Bioethics. 2016; 7(4):251-259.
- Carman KL, Dardess P, Maurer M, Sofaer S, Adams K, Bechtel C, et al. Patient and family engagement: A framework for understanding the elements and developing interventions and policies. Health Affairs. 2013; 32(2): 223-231.
- Reti SR, Feldman HJ, Ross SE, Safran C. Improving personal health records for patient-centered care. J Amer Medical Inform Assoc. 2010; 17(2): 192-195.
- Tanigawa K, Tanaka K. Emergency medical service systems in Japan: Past, present, and future. Resuscitation. 2006; 69(3): 365-370.
- Hori S. Emergency Medicine in Japan. Keio J Med. 2010; 59(4): 131-139.
- Provalis Research. Qualitative Data Analysis Software, Mixed Methods Research Tool Provalis 2019.
- Coiera E, Tombs V. Communication behaviours in a hospital setting: An observational study. BMJ. 1998; 316(7132): 673-676.
- Zibrowski E, Shepherd L, Sedig K, Booth R, Gibson C. Easier and Faster Is Not Always Better: Grounded Theory of the Impact of Large-Scale System Transformation on the Clinical Work of Emergency Medicine Nurses and Physicians. JMIR Human Factors. 2018; 5(4): e11013.
- Eagle K, Ryan C. Mind the gap: The potentially incapable patient who objects to assessment. Australian Law J. 2012; 86: 685-696.
- Thompson ML. Characteristics of information resources preferred by primary care physicians. Bulletin of the Medical Library Assoc. 1997; 85(2): 187-92.
- Owolabi K. Clinical informatics tools for healthcare quality improvement: A literature review. Inkanyiso: J Humanities Social Sci. 2018; 10(1): 74-89.
- Jilka SR, Callahan R, Sevdalis N, Mayer EK, Darzi A. Nothing about Me without Me: An Interpretative Review of Patient Accessible Electronic Health Records. J Med Internet Res. 2015; 17(6): e161.
- Caine K, Hanania R. Patients want granular privacy control over health information in electronic medical records. J American Med Inform Assoc. 2013; 20(1): 7-15.
- European Parliament. Regulation (EU) 2016/679 of the European Parliament and of the Council. EUR-Lex 2016.
- Morris K, Yamamoto G, Hiragi S, Ohtera S, Sakai M, Sugiyama O, et al. Designing an authorization system based on patient privacy preferences in Japan. Studies Health Technol Inform. 2018; 247: 71-75.
- Ming L, Shucheng Y, Kui R, Wenjing L. Securing personal health records in cloud computing: Patient-centric and finegrained data access control in multiowner settings. . LNICST. 2010; 5: 89-106.
- Patton MQ. Qualitative Research & Evaluation Methods. SAGE Publications; 2015: 832.
- Perera G, Holbrook A, Thabane L, Foster G, Willison DJ. Views on health information sharing and privacy from primary care practices using electronic medical records. Int J Med Inform. 2011; 80(2): 94-101.
- Ayatollahi H, Bath PA, Goodacre S. Accessibility versus confidentiality of information in the emergency department. Emergency Medicine Journal. 2009; 26(12): 857-860.
- Alaqra AS, Fischer-Hübner S, Framner E. Enhancing privacy controls for patients via a selective authentic electronic health record exchange service: Qualitative study of perspectives by medical professionals and patients. J Medical Internet Res. 2018 12; 20(12): e10954.
- Cherns A. The Principles of Sociotechnical Design. Human Relations. 1976; 29(8):783-792.
- Wilson TD. Information sharing: An exploration of the literature and some propositions. Inform Res. 2010; 15(4): 1-5.