Are EHR Standards Capable of Handling the Challenges of Smart Healthcare? Data-Level Research
2 Department of Information Technology, Techno Main Salt Lake, Maulana Azad University of Technology Kolkata, India
Received: 02-Jul-2022, Manuscript No. ejbi-22-69636; Editor assigned: 04-Jul-2022, Pre QC No. ejbi-22-69636(PQ); Reviewed: 18-Jul-2022 QC No. ejbi-22-69636; Revised: 20-Jul-2022, Manuscript No. ejbi-22-69636(R); Published: 27-Jul-2022, DOI: 10.24105/ejbi.2022.18.7.69-72
Citation: Mukherjee N (2022). Are EHR Standards Capable of Handling the Challenges of Smart Healthcare? Data-Level Research. EJBI. 18(7):69-72.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact submissions@ejbi.org
Abstract
Electronic Health Records (EHRs) are required for maintaining and using medical data. Many internationally well accepted EHR; EHR-S standards are available in the medical domain. There are various related health data standards as well. All these standards have specific advantages and disadvantages. Standard making process is an iterative process and the standards are still evolving. Though several important standards have been proposed during the last few decades, one major problem of these EHR standards is that they are not defined according to scope, scale and context. Computerized processes require specific definitions of medical terms and such terms are not very generic in respect of usage in different countries. There are also many aspects of evaluation of health data standards. In this paper, EHRs and other related standards, their usage, shortcomings etc. are studied in the context of data storage, data model and exchange of data formats. Suitability of the standards for smart environments is also explored with an objective to find a suitable presentation, organisation and storage of health data generated through smart health care applications.
https://transplanthair.istanbul
https://hairclinicturkey.co
https://hairclinicistanbul.co
https://besthairtransplant.co
https://hairtransplantistanbul.co
Keywords
EHR-S, Health data standards, Interoperability, Data model
1.Introduction
Health records in paper are not preferred any more anywhere for known reasons like errors, no option for interoperability between different care giving service providers, problems related to maintainability and longevity etc. EHRs are being used in different parts of the world so that maintenance and sharing of medical records become easier for care givers. Privacy and security are also other important requirements to be maintained. Electronic Health Record or EHR contains basic and medical details of patients such as demographic data, medical parameters, reports of laboratory tests, different images related to different tests, treatment details, visit or encounter details etc. at different instants of time. EHRs are primarily used for storage, representation and communication of health data. It is also used to show the relationship between the different components of health data. EHR system or EHR-S provides the software support to enter, modify, view or analyse, and also to provide support for maintenance of EHR. It can be used for decision support to doctors. It also provides support to other related activities [1].
However, with increased use of Internet of Things (IoT) based e-health and m-health applications in healthcare, such as continuous monitoring of patients remotely over the Internet, question arises whether EHRs are suitable for handling smart environments [2].
Though several important standards of EHR have been proposed during the last few decades, one major problem of these EHR standards is that they are not defined according to scope, scale and context. Computerized processes require specific definitions of medical terms and such terms are not very generic in respect of usage in different countries. Moreover, these standards of EHR do not specify explicitly how health data will be stored for optimum performance in case of data retrieval. A high level concept for data storage is used in some of the standards. For example, in case of EN13606, le, folder, section etc. are defined. But, whether such high level concepts are useful for capturing, defining and retrieving health data has never been studied. In particular, when most of the smart environments intend to use NoSQL databases, healthcare applications, which still use EHRs, have never attempted to find a suitable technique to map the EHRs to NoSQL databases [3-5].
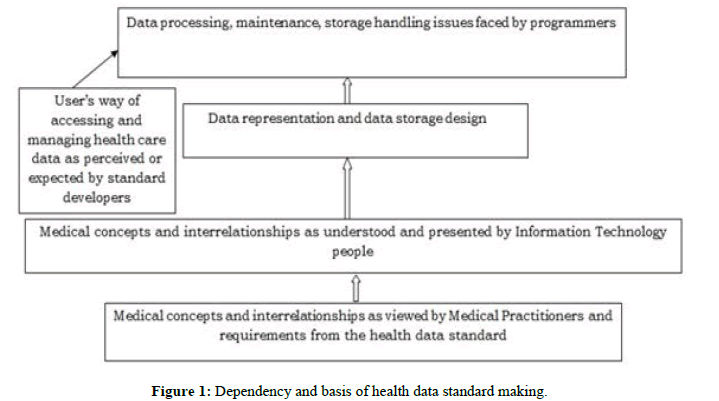
In the above context, coverage, scale and scope and storage performance can be points of study in defining medical records. This paper aims at studying various EHR standards in the light of developing smart healthcare information systems. In the earlier surveys targeting standards of EHR, EHR-S have been studied from various perspectives quality of information, systems and services, intention of usage, use, satisfaction of user, benefits of EHR, different factors to influence implementation of EHR, EHR-S etc. [6]. On the contrary, in this paper, a study of EHR and other supporting health data standards is undertaken in the context of data storage, data representation and data handling (Figure 1).
The following standards and their advantages and shortcomings are studied in this paper:
• ISO 13606
• OpenEHR
• HL7- Health Level Seven Reference Information Model (RIM), Continuity of Care Data (CCD), Clinical Document Architecture (CDA), Fast Healthcare InteroperabilityResources (FHIR), CIMI (Clinical Information Modeling Initiative)
• Unified Medical Language System (UMLS)
• Systematized Nomenclature of Medicine (SNOMED)
• Logical Observation Identifiers Names and Codes (LOINC)
• International Classification of Diseases (ICD)
Initially the standards are studied from the resources provided by the standard making bodies and research papers. In the next step, the usage and feedback from different research studies related to implementation of these standards are included. The paper also studies how these standards are used in research. Also some white papers published in this context are referred. In the second section of this paper, a brief overview of different standards for EHR and other related clinical standards is given. In the third section, evaluation aspects of EHR and EHR-S are discussed. In the fourth section, some experiences of implementation of the standards are described on the basis of some research works. In the fifth section, a discussion is made based on suitability of the standards for smart environments. In the sixth section, the paper is concluded with reference to future direction of the work [7,8].
ISO 13606: Standard for EHR extracts, Follows dual model architecture, model of information and model of reality, Archetypes and ADL available.
Open HER: Open Standard for EHR and EHR-S, Wider scope in comparison to ISO 13606, Open to change, update, Archetypes available through archetypes are not full proof for example diabetes.
UMLS: Provides knowledge sources, software tools for biomedical, health data, work with patient records, scientific literature, guidelines, and public health data.
HL7: Standard for communication of medical data between two systems can be used for message and communication, support standard needed for standards of EHR and EHR-S.
SNOMED CT: Repository of biomedical terminologies, has identifier terms, depicts concepts, descriptions and relationships, support standard.
LOINC: Universal coding system for identifying laboratory and clinical observations, measurements, a support standard, indispensable for EHR and EHR-S.
ICD: International standard diagnostic classification of for clinical use, indispensable for implementation of EHR and EHR-S.
2. EHR and EHR-S Evaluation Factors and Findings
There are different dimensions of evaluation of impact of EHR usage. It can be evaluated on the basis of information quality, perspective of evaluation perception based, quantitative or qualitative, objective data based, effect of dealing with huge amount of data, features found, problems found etc. Another dimension of evaluation can be system quality. Some people are comfortable and others are not with the provided user interfaces. Sometimes clinicians are not happy entering so much of data instead of treating patients. Lastly there are factors of service quality- interoperability concerns that include difficulties with IT support fulfilling urgent requests and sometimes lack of IT support [9].
Portability: Portability is an important feature for implementation of such standards. Different users have different requirements, expectations and needs that EHR must be able to deliver. Usage of EHR and EHR-S brings changes to documentation practices and it is responsible for medium or low response for adoption and usage satisfaction of the standard [10]. It is found that organization of such huge data is a key point in influencing information retrieval and usage. Interoperability of EHR systems into existing technology infrastructure is also an important issue [11]. EHR systems were found well integrated but communication with the physician in the outside world was difficult. The scope of usage of mobile health and telehealth are not well explored in some countries. Patients of some places directly use and believe that web portals are of great benefit in chronic care management. But these portals are not well designed and integrated with other EHR systems properly. Patients are generally concerned over the privacy, confidentiality of health data and usefulness, usability of Personal Health Record [12].
Result
Standards are indispensable: Healthcare application needs to use internationally accepted EHR, EHR-S and some other support standards starting from the fundamental design of the application.
Drawbacks: Standards do not cover everything, for example it does not specify data store design or guide implementation procedure implicitly. Archetypes are not t to be used in all scopes, scales, context and countries.
Adaptability: The standards are not made keeping in mind that the health care application may have to work in a very low scale with limited infrastructure, such as while handling an accident or natural calamity. Sometimes, again the standards are failing where explicit details are needed with respect to a particular medical problem such as diabetes.
Difficulties in using the standards: It has been reported extensively that health care people spend most of their time handling the difficulties of storing health data electronically.
Internationally acceptable standards: Like internationally accepted standards in other domains, there must be one standard to be followed everywhere recommended by medical practitioners.
Interoperability: Due to the difference in the data models of different standards, there is chance of loss of data or incompleteness in expressing medical data in one standard when converted from another standard.
Approval of clinicians: Standards must be understood and agreed upon by clinicians. Thus, during usage, clinicians must agree with the way they perceive the implementation of the standard. They must come across the everyday used clinical terms.
Usage in different situations: The competence of a standard must be tested by using it in as many situations as possible. For example OpenEHR has the openness to be used repetitively and to be modified to become better than before.
Quality of standards: Design of health data standards is at times very generic and at times too specific. Generally these standards are defined in a very generic manner so that almost all situations can be covered. However sometimes, standards are too specific and applicable to a particular application and a particular scope and a particular country.
Use of modern technologies: Specifications of health data standards do not incorporate cloud, streaming data coming from sensors. Proprietary data obtained from a device that captures health data, must be made available for health data storage and reused in a format that is accepted.
Role of ontology: ISO 13606 uses ontology for its archetypes. HL7 V3 Release 1 has privacy and security ontology FHIR uses ontology to make its resources shareable and to make validation of data possible. It is also used so that it can be combined with other health related ontologies to build a health care application.
4. Application Development
There are various aspects of EHR definition and usage. There is a need to define medical concepts and their interrelationships for data storage, data handling and maintenance issues. There is another aspect that covers the medical terminologies and their interrelationships with synonyms of different standards. The difference between medical terminologies and concepts is how care people use data and how people of information technology understand the interrelationships among the different medical concepts so that the data model and in future the data storage can be meticulously designed to optimize performance. The third aspect deals with the domain where every day people store a record or an image or a test data in les etc., i.e. how people store, use, modify, access data every day. There is another perspective that deals with how programmers will process such data. The interrelationships among the different representations of the different aspects are to be defined. Ontology uses open world concept and it is the repository of information. Information model that is used to develop an application uses closed world concept. It needs a theoretical knowledge repository like ontology.
Conclusion
This paper presents a survey of health data standards. It argues that ontology should be defined to capture the domain knowledge to support health data standards. A global health data standard should adapt to scale, scope and countries. Such health data standard must manage normalized data sources or its implementation. It must also work with sensed streaming data, cloud, and other modern technologies. In future, effort must be given to come up with one acceptable standard just like in most technological domains. Otherwise, the process of conversion from one standard format to another standard format must be made full proof, loss less and easily possible. There must be a balance between the level of generality and the level of details covered. This is because medical concepts and terminologies are not easily available or graspable to people belonging to technical domain or for computer processes. This is also because; complete infrastructure for care process may not be available at the time of medical emergency and in remote places.
References
- Nguyen L, Bellucci E, Nguyen LT. Electronic health records implementation: an evaluation of information system impact and contingency factors. Int J Med Info. 2014; 83(11):779-796.
- Martinez-Costa C, Menarguez-Tortosa M, Fernandez-Breis JT. An approach for the semantic interoperability of ISO EN 13606 and OpenEHR archetypes. J Biomed Informatics. 2010; 43(5):736-746.
- Stan O, Miclea L. Local EHR management based on FHIR. In2018 IEEE International Conference on Automation, Quality and Testing, Robotics (AQTR) 2018: 1-5.
- Lozano-Rubi R, Carrero AM, Balazote PS, Pastor X. OntoCR: A CEN/ISO-13606 clinical repository based on ontologies. J Biomedical Informatics. 2016; 60:224-233.
- Lee D, Cornet R, Lau F, De Keizer N. A survey of SNOMED CT implementations. J Biomedical Informatics. 2013; 46(1):87-96.
- Friedman DJ, Parrish RG, Ross DA. Electronic health records and US public health: current realities and future promise. Ame J Public Health. 2013; 103(9):1560-1567.
- El-Sappagh S, El Mogy M, Riad AM. A standard fragment of EHR relational data model for diabetes mellitus diagnosis. In2014 9th International Conference on Informatics and Systems. 2014.
- Papez V, Denaxas S, Hemingway H. Evaluating OpenEHR for storing computable representations of electronic health record phenotyping algorithms. In2017 IEEE 30th International Symposium on Computer-Based Medical Systems (CBMS) 2017: 509-514.
- Almeida J, Frade S, Cruz-Correia R. Exporting data from an openEHR repository to standard formats. Procedia Technology. 2014; 16:1391-1396.
- Bae S, Lee DY, Kim IK. Rendering Problem-Oriented CCD for chronic diseases. In2017 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC). 2017: 4277-4280.
- Bosca D, Maldonado JA, Moner D, Robles M. Automatic generation of computable implementation guides from clinical information models. J Biomedical Informatics. 2015; 55:143-152.
- Martinez D, Otegi A, Soroa A, Agirre E. Improving search over Electronic Health Records using UMLS-based query expansion through random walks. J Biomedical Informatics. 2014; 51:100-106.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref